ISO/HL7 10781 - Electronic Health Record System Functional Model, Release 2.1
0.14.0 - CI Build
ISO/HL7 10781 - Electronic Health Record System Functional Model, Release 2.1
0.14.0 - CI Build
ISO/HL7 10781 - Electronic Health Record System Functional Model, Release 2.1 - Local Development build (v0.14.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the Directory of published versions
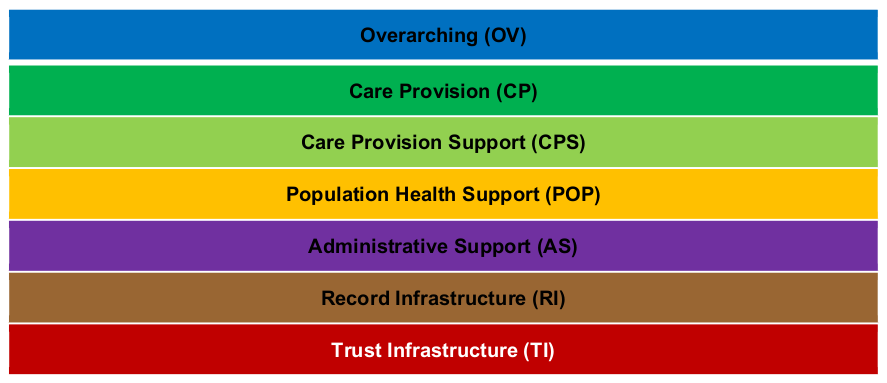
The EHR-S Functional Model is composed of a list of functions, known as the Function List, which is divided into seven sections: Overarching, Care Provision, Care Provision Support, Population Health Support, Administrative Support, Record Infrastructure and Trust Infrastructure.
Within the seven Sections of the Functional List the functions are grouped under header functions which each have one or more sub-functions in a hierarchical structure.
Below is a summary description of each of the seven sections:
While the Functional Model contains all reasonably anticipated EHR-S functions, it is not itself intended as a list of all functions to be found in a specific EHR-S or implementation thereof. Functional Profiles offer a method to constrain EHR-S FM functions and conformance criteria to an intended use. In the aggregate, the EHR-S FM is intended to include the superset of functions from which a profile subset can be generated. This subset illustrates what is needed within an EHR-S. Only a subset of all EHR-S FM functions will apply to any particular EHR-S Functional Profile (FP).
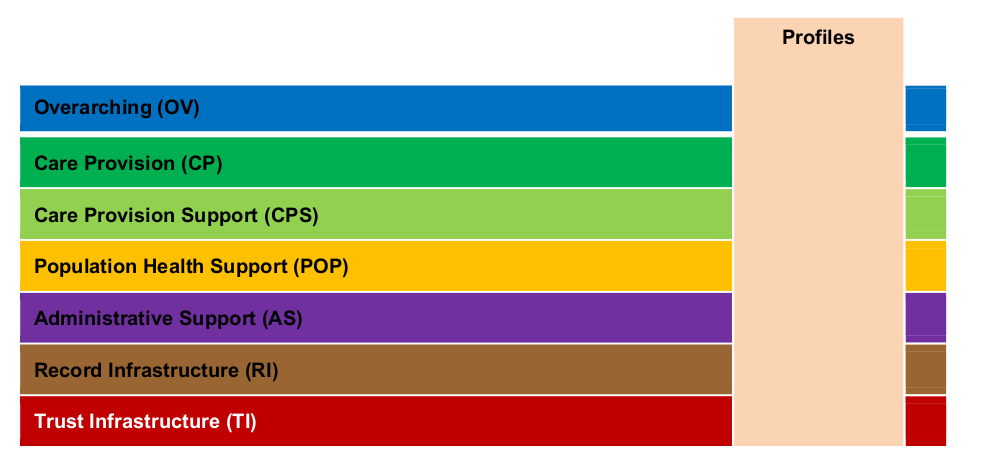
Figure 2 shows that a profile would include all 7 sections of the Functional Model, however it may not be necessary to include all the functions and criteria within each section. A profile may include additional functions and criteria to meet the requirements of the particular profile domain or subject area. The Conformance Clause is a high-level description of what is required of profiles and implementations. It, in turn, refers to other parts of the standard for details. The Conformance Clause describes concepts critical to the understanding and implementation of the Functional Model, such as: ‘What is a profile? What are Conformance Criteria? Or how do you know what is mandatory versus optional?. A Conformance Clause can also provide a communication between the implementers (producers) and users (buyers) as to what is required, and gives meaning to the phrases, “conforming profile” and “conforming EHR system”. Additionally, it serves as the basis for inspection, testing and/or certification activities which may be performed by organizations external to HL7. Refer to the Conformance Clause, for additional information related to the rules for selecting and adding Conformance Criteria in the development of a Functional Profile.
The EHR-S Function List is a list (superset) of functions organized into discrete sections. Functions describe the behavior of a system in user-oriented language so as to be recognizable to the key stakeholders of an EHR-S.
EHR-S functions can be used to:
Each function in the HL7 EHR-S Functional Model is identified and described using a set of elements or components as detailed below.
| ID | Type | Name | Statement | Description | Conformance Criteria |
|---|---|---|---|---|---|
| CP.1 | H | Manage Clinical History | Manage the patient’s clinical history lists used to present summary or detailed information on patient health history. | Patient Clinical History lists are used to present succinct “snapshots” of critical health information including patient history; allergy intolerance and adverse reactions; medications; problems; strengths; immunizations; medical equipment/devices; and patient and family preferences. | |
| CP.1.4 | F | Manage Problem List | Create and maintain patient-specific problem lists. | A problem list may include, but is not limited to chronic conditions, diagnoses, or symptoms, injury/poisoning (both intentional and unintentional), adverse effects of medical care (e.g., drugs, surgical), functional limitations, visit or stay-specific conditions, diagnoses, or symptoms… | |
| CP.1.4 | C | 1. The system SHALL provide the ability to manage, as discrete data, all active problems associated with a patient. | |||
| CP.1.4 | C | 2. The system SHALL capture and render a history of all problems associated with a patient. | |||
| CP.1.4 | C | 3. The system SHALL provide the ability to manage relevant dates including the onset date and resolution date of problem. |
Table 2: Function List Example
This is the unique identifier of a function in the Function List (e.g., CP.1.1) and uniquely identifies the function. The Function ID also serves to identify the section within which the function exists (CP = Care Provision Section) and the hierarchy or relationship between functions (CP.1.1 is at the same level as CP.1.2, CP.1.1 is also a parent of CP.1.1.1 and child of CP.1. In many cases the parent is fully expressed by the children. NOTE: For a detailed discussion and graphic of the parent and child relationship, see 6.6.1 Hierarchical Structure in Chapter 6, Conformance Clause.)
This is an indication of the line item as being a Header (H), Function (F) or Conformance Criteria (C). The Tag (T) is used to identify a new section in the spreadsheet and its related functions in the spreadsheet. A Tag has no directly associated Functions or Criteria.
This is the name of the Function and while expected to be unique within the Function List; it is not recommended to be used to identify the Function without being accompanied by the Function ID. Example: Manage Medication List
This is a brief statement of the purpose of this function. While not restricted to the use of structured language that is used in the Conformance Criteria (see below); the Statement identifies the purpose and scope of the function. Example: Create and maintain patient-specific medication lists.
This is a more detailed description of the function, including examples if needed. Sample Description: Medication lists are managed over time, whether over the course of a visit or stay, or the lifetime of a patient. All pertinent dates, including medication start, modification, and end dates are stored. The entire medication history for any medication, including alternative supplements and herbal medications, is viewable. Medication lists are not limited to medication orders recorded by providers, but may include, for example, pharmacy dispense/supply records, patient-reported medications and additional information such as age specific dosage.
Each function in the Function List includes one or more Conformance Criteria. Conformance Criteria, which exist as normative language in this standard, define the requirements for conforming to the function. The language used to express a conformance criterion is highly structured with standardized components with set meanings. The structured language used to define Conformance Criteria in the Function List are further specified in the Conformance Section and Glossary Section.